Tell CareWay exactly how you want your notes to be generated!
The template builder in CareWay is an essential tool to ensure the relevance and quality of your clinical notes. Designed to adapt to the needs of each consultation or report type, it generates note templates that faithfully reflect your expectations and constraints. By adding targeted instructions, you can improve the clarity and consistency of your notes while significantly reducing the number of edits needed in the final version.
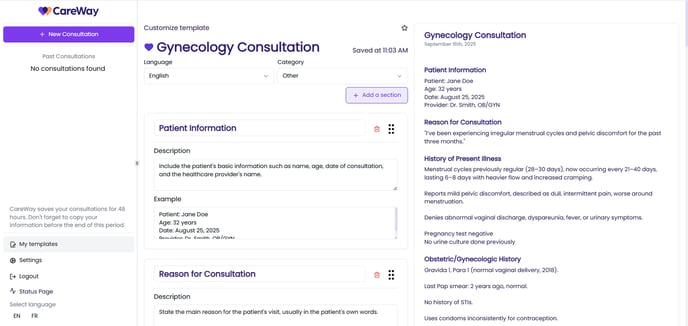
Step 1 – Create Your Custom Templates
Start by creating your own note templates using the template builder.
Step 2 – Add Clear Instructions for the AI
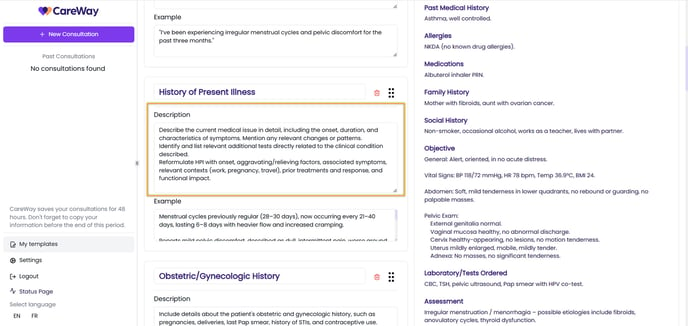
In edit mode of a note template, the Description field of each section allows you to give the AI precise instructions for generating the note. You can use it to:
-
Define the structure of the note according to your clinical habits.
-
Add conditional rules (e.g., “If I mention X, add Y”).
-
Indicate the purpose of the section (e.g., summary, plan, justification).
Recommended Instruction Styles
-
Clear and direct: Short and precise; no ambiguity for the AI.
Example: “List all lab results mentioned, with test name, value, and units.” -
Contextualized: The context (specialty + type of follow-up) guides the response format.
Example: “In cardiology, for a hypertension follow-up visit, present blood pressure with patient position and compare it to the last visit.” -
Behavioral (if… then): Explicit conditional rule, clearly defined behavior.
Example: “If a lab result is outside the reference range, flag it and add one sentence of clinical interpretation.” -
Outcome-oriented: Expected result well defined (form + content).
Example: “Generate a concise three-line summary that includes the chief complaint, one key objective finding (exam or lab), and the plan.”
Examples of Effective Instructions for Specific Contexts
-
Laboratory values and interpretation
Include for each lab parameter: full name, numeric value with SI units, reference range if available, date/time of collection, and a one-sentence clinical interpretation (e.g., “ferritin 18 µg/L, low, consistent with iron deficiency”). Never summarize only as “normal/abnormal.” -
Complete medication list and changes
List for each drug: generic name, dose, form, route, frequency, indication, start/stop date, adherence, side effects, and any changes decided today with justification. Also include allergies and reactions. If a dimension is missing, request clarification. -
Medication discussion
Ensure the Plan and Recommendations section includes any discussion about medication, even when no prescription was made. Specify whether pharmacological treatment was considered, discussed, accepted, refused, or deferred. -
Vital signs and measurements with units
Document BP (position, arm), HR, RR, Temp, SpO₂, height, weight, BMI, and waist circumference. Include units and context (sitting/lying). Highlight critical values and trends if serial measurements are available. -
Structured history of present illness (HPI)
Reformulate HPI with onset, aggravating/relieving factors, associated symptoms, relevant contexts (work, pregnancy, travel), prior treatments and response, and functional impact. -
Physical exam by systems
Document positive and relevant negative findings by system. Include specific maneuvers (e.g., Murphy’s sign, Ottawa ankle rules) and standardized gradings (e.g., muscle strength 4/5). Avoid using “normal” without detail. -
Traceable investigation plan
For each test/imaging, specify clinical indication, priority, location (if known), consent/explanations given, and connection to working diagnoses. Include standardized codes if available (ICD-10-CA/CCI/SNOMED CT). -
Therapeutic plan and follow-up
Describe pharmacological and non-pharmacological treatments, goals, safety/monitoring parameters, patient education, and red flags for urgent reassessment. Document the follow-up date/location and responsible professional. -
Patient instructions (teach-back)
Summarize in the format: “I explained that…” + “The patient restated that…”. Record handouts/links provided, patient preferences, and anticipated barriers. -
Consent and confidentiality
Note type of consent (implied/explicit), purpose (collection, use, disclosure), discussion of risks/benefits/alternatives, and any patient-requested restrictions, in accordance with PHIPA/PIPEDA. -
Care coordination and consultations
Indicate specialists/contacts involved, communication method (eConsult, phone, letter), clinical question summary, information transmitted, and patient agreement. -
Legal context and minimum documentation requirements
Ensure the note includes: patient identifiers (name, DOB, HCN if applicable), date/time of encounter, clinician and site ID, and updated CPP/summary when necessary. -
Social, risks, and determinants of health
Capture tobacco, alcohol, substances, housing, food security, employment, social support, transportation. Indicate relevance to the complaint and treatment decisions. -
Language and interpreter
Document preferred language, interpreter use (name/ID/platform), or presence of a companion, as well as the impact on consent and understanding. -
Teleconsultation
Record modality (phone/video), connection quality, exam limitations, patient identification measures, location of each party, and consent specific to telemedicine. -
Pregnancy, pediatrics, and dosing
If pregnant/breastfeeding or pediatric: include relevant obstetric info (GA), current weight (kg), dose calculations (mg/kg), and references if cited. -
Record security and retention
Confirm that all document exchanges are secure. Note any access or correction requests and actions taken. Respect transfer and retention policies. -
Scores and decision rules
Include score name (e.g., Wells, CHA₂DS₂-VASc), key variables, numeric result, and clinical implication (e.g., “Wells 5 = moderate probability → D-dimer/CT”). -
3-line clinical summary
End with “In summary:” followed by:
1. problem/situation,
2. key evidence (symptoms, exam, labs with figures),
3. decision/plan and follow-up.
Optimized for quick review and care continuity.
-
Mood and affect
Document separately the patient’s reported mood (e.g., sad, anxious, irritable) and the clinician’s observed affect (e.g., congruent, flat, labile). Avoid vague single terms like “normal.” -
Sleep, appetite, and energy
Include details on sleep, appetite, and energy, even if stable, as these are key for longitudinal mental health monitoring. -
Social and occupational functioning
Describe global functioning (work, studies, relationships, autonomy), noting any recent changes. Include details even if secondary to the main complaint. -
Adherence and side effects
For each psychotropic treatment: note adherence, subjective side effects, and perceived efficacy. If the patient self-modified or stopped medication, document clearly. -
Complete active problem list
Generate a structured list of all active health issues discussed during the consultation, even if stable or secondary. For each, note evolution, current treatment, and today’s decisions or changes. -
Medication, interactions, and adherence
Document all medications (prescribed, OTC, natural) with dose, frequency, indication, adherence, and side effects. Include recent changes, adjustments made today, and any interactions or contraindications discussed. -
Functionality and geriatric determinants
Systematically include functioning (ADLs, IADLs, mobility, cognition, falls, continence, nutrition, social support). Note any change since last visit and impact on care plan. -
Negative findings mentioned
In the Exam section, also include explicitly assessed negative findings (e.g., “No major anxiety symptoms,” “No abnormal neurological signs,” “No aggressive behaviors observed”). Documenting what was checked and found non-significant supports clinical reasoning.